The ‘Skinny’ on Cancer Awareness

Increasing cancer awareness and the proliferation of education is probably more important now than it ever has been. This is especially salient when confronting the changing picture shown by research from the American Cancer Society. Their most recent estimate shows that “In 2017, nearly 13% of all cancers diagnosed in adults ages 20 and older will be rare cancers…” A rare cancer is defined in their most recent report “as a cancer with fewer than 6 cases per 100,000 people per year”. (https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2017.html)
In the American Cancer Society’s findings last year, they showed a decrease in cancers such as Colon Cancer, yet showed an increase in other types such as liver, tongue and kidney, as well as some types of leukaemia. (https://www.cancer.org/latest-news/cancer-statistics-report-death-rate-down-23-percent-in-21-years.html#helpful_resources)
The ‘pictures painted’ by both sets of research from 2016 and most recently in 2017 show that cancer is a ‘changing animal’. This emphasizes how important cancer awareness is for all concerned; both healthcare professionals and the general public.

One of the greatest challenges for a physician, is finding the right communicative approach when giving a patient a cancer diagnosis. All patients have different reactions to devastating news. Some patients are more emotive, others may be emotionally numb, and it may take them a lot longer to accept the bad news.
Luckily there is a ‘helping hand’ for both patients and physicians offered by a new book called ‘Living with Cancer’. This book is the collaboration of Chief of Hematology and Oncology, David Ryan and Vicky Jackson, Chief of Palliative Care, both from Massachusetts General Hospital. (The book is also coauthored with medical writer Michelle Seaton). In the words of Dr. Jackson, “I hope this book is like a decoder ring for people, because it is surreal to have a cancer diagnosis. It doesn’t matter how capable you are in your professional world, you have no clue about the terms you’re going to hear or what it’s going to feel like.” (https://www.bostonglobe.com/magazine/2017/05/17/two-mgh-doctors-offer-step-step-advice-for-living-with-cancer/rC0eryFm4VbgffHQfsNLLJ/story.html)
Twining the approach of Palliative Care with Oncology
Perhaps what makes ‘Living with Cancer’ a unique book is its focus. The book’s main emphasis is on patients’ symptom management and the patient’s emotional wellbeing from the “front end of cancer treatment”. This differs completely with the traditional approach where it is just introduced “with patients at the end of life”. This integrated approach of concentrating on patients’ symptom management and their emotional wellbeing, has received support from research by Dr. Jennifer Temel. Dr. Temel discovered that when this approach was applied, patients experienced lower levels of depression and lived longer.
One of the disadvantages of the traditional medical approach to patients, says Dr. David Ryan; is that the Oncology MD is “not spending as much time on side effects affecting their quality of life — like can they tie their shoes? — whereas somebody who’s focused on symptom management (like a Palliative professional) is”. By interweaving the approaches of Palliative care with Oncology medicine, the oncology physician may increase their patients’ chances. ((https://www.bostonglobe.com/magazine/2017/05/17/two-mgh-doctors-offer-step-step-advice-for-living-with-cancer/rC0eryFm4VbgffHQfsNLLJ/story.html)

As Dr. David Ryan has seen it is important that patients are empowered to ask questions, it is also critical for patients to feel comfortable talking with their physician. Many patients don’t tell their oncologist everything as Ryan says, “They’re trying to put on their best face for me because they want passing grades”. It’s also important to emphasize to the patient that they are not a number and don’t make up an average. Each case is unique and needs to be treated that way. As Dr. Vicky Jackson says new treatments like immunotherapy (treatments that employ the body’s own immune system to fight cancer) may not always be effective for everybody. “For a small percentage (of patients), the cancer melts away. For most people nothing happens. And for a small percentage, it’s deadly.”
The Shared Decision Approach: Can joint active decision making help patient oncology care?

Another key approach focusing on improving patient engagement is called the shared decision approach. This refers to the joint discussion between the patient and physician for the purpose of reaching a shared healthcare choice. This can involve decision making about screening and diagnostic tests, self- management, or medications. As part of this shared decision approach, the physician may want to introduce decision aids to their patients. These range from DVDs to interactive websites. A 2012 Cochrane review discovered that patients who use patient aids have broader knowledge of treatment options and have more realistic expectations of potential benefits and risks. They are also more likely to actively participate in the decision making process. (https://powerfulpatients.org/2017/05/23/mapping-the-patient-information-journey/Mapping)

Another growing trend with patients is using ‘peer to peer’ healthcare. This is where a patient searches for certain Facebook groups or online forums of people who share similar predicaments. There are even Twitter groups which physicians take a part in. This trend has created a new breed of patient, the ‘e-patient’ (a term created by Dr. Tom Ferguson). This type of patient is more motivated to find the best resources, treatment centers, and the most up to date research. (https://powerfulpatients.org/2017/05/23/mapping-the-patient-information-journey/Mapping)
So far I have focused on relationship between physicians and their patients. Now I will discuss technologies and recent research that can help oncology professionals do their job more effectively.
Advances in Technology and Research: Is there a cure for Cancer on the horizon?
In all fields of healthcare, new research and new technologies are being developed almost ‘as we speak’. One example is the spread and popularity of digital technology. New technology is being developed that will transform current cancer care methods on the market. These types of personalized oncology are being made available by start-ups and companies such as SmartPatients and Foundation Medicine. (https://medicalfuturist.com/the-most-exciting-medical-technologies-of-2017/)
Both Foundation Medicine and SmartPatients are two companies with different visions. Foundation Medicine aims to introduce cancer genomics into cancer care. These technologies provide data related to patient-specific cancer treatments. This information is based on DNA-tests. SmartPatients vision takes a different approach by looking at how to improve patient engagement through joining an online community.

Significant progress has also been made in the field of immunotherapy. There is definitely potential for immunotherapy to become the next progressive step in treating cancer. Liquid Biopsy ‘was all the rage’ in 2016 and is now becoming increasingly available worldwide. Liquid Biopsy is defined by www.rouche.com as “a simple and non-invasive alternative to surgical biopsies which enables doctors to discover a range of information about a tumor through a simple blood sample. Traces of the cancer’s DNA in the blood can give clues about which treatments are most likely to work for that patient.” (https://www.roche.com/research_and_development/what_we_are_working_on/oncology/liquid-biopsy.htm )
Despite its awesome promise of avoiding more invasive surgical biopsies, its limitations are well known. One example of its limitations is that blood samples need to be obtained before for a chemotherapy. Another example is it is also very difficult to detect cancer cells using this method.

New Zealand, Auckland is the location where some of the most pioneering research is taking place. Auckland engineering Professor Steve Henry has found a totally innovative and new way to potentially cure cancer. His ground-breaking research has managed to secure a spot in the world-renowned Johnson and Johnson Innovation Centre JLABS, in Houston.
Professor Henry has created a molecule that can be painted onto a surface. This has the effect of changing the surface, and thus the way it acts and interacts. As Professor Henry says, “We can engineer this molecule to do just about anything you want it to do.”
(https://www.newshub.co.nz/home/health/2017/04/kiwi-made-technology-could-cure-cancer.html)
Professor Henry and his team have found the same method can be used to change the surface of a cancer cell. By adding this biological paint he calls Kode Technology paint, it changes the surface, thus helping the immune system to recognize these cancer cells as foreign tissues. The immune system is then able to destroy them.
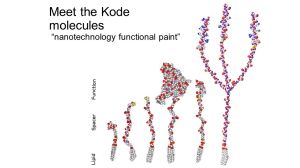
Henry says, “We’ve made a biological paint which can be injected into a cancer cell, and it will teach your body how to recognize your own cancer, and theoretically you could inject a single tumor and all your tumors will go.” Human clinical trials begin next year. The possibilities for this novel solution are almost endless. (https://www.newshub.co.nz/home/health/2017/04/kiwi-made-technology-could-cure-cancer.html)
The next generation of Henry’s Kode Technology biological paints will minimize implant infections. This is easily done by coating the surface of the knee, or hip implant. This makes it self-sterilizing. Other novels uses include: creating bandages that heal a wound faster and make-up that guards the skin from damaging pollutants.
Professor Henry and his team have been working on this and other Kode Technology for the past 20 years. The future for these biological paints and other Kode Technology is bright, especially now having secured the support and added resources of JLABS.(https://www.cancer.gov/news-events/cancer-currents-blog/2017/nci-almanac-drug-combinations)
What does the future hold for Cancer Care?

In conclusion, cancer is probably one of the most changing diseases that there is in the healthcare world. As can be seen from research presented by American Cancer Society, statistics show a completely different picture year after year.
On a more positive note, there are firms such as Foundation Medicine that have introduced data related to patient-specific cancer treatments. One of the most novel solutions, and one with the most exciting potential is Steve Henry’s Kode Technology biological paint. When painted onto the surface of cancer cells, it changes the surface, enabling the immune system to fight them. The creativity and pioneering spirit displayed by New Zealand based Professor Steve Henry gives renewed hope that the fight against cancer will one day be won.
